Arthritis Pain / Joint Pain
Joints form the connections between bones. They provide support and help you move. Any damage to the joints from disease or injury can interfere with your movement and cause a lot of pain. Joint pain is extremely common. About one-third of adults report having joint pain within the past 30 days.
Knee pain is the most common complaint, followed by shoulder and hip pain, but joint pain can affect any part of your body, from your ankles to your shoulders. As you get older, painful joints become increasingly more common.
Joint pain can range from mildly irritating to debilitating. It may go away after a few weeks (acute), or last for several weeks or months (chronic). Even short-term pain and swelling in the joints can affect your quality of life.
Many different conditions can lead to painful joints, including Arthritis, bursitis, strains, sprains, and other injuries. Among these Arthritis is most common causes.
Arthritis is a non-specific term for inflammation of joint. Inflammation is the body’s first reaction to injury. When the joint is inflamed due to some internal of external injury it is called arthritis.
In the case of joint inflammation (or arthritis) the following changes occur:
In response to injury, nonspecific immune system is activated (immune system is the body’s defense system.) It may be activated by injured tissue debris in or around the joint. Sometimes the immune system is wrongly activated without any injury.
When immune system is activated, there is increased blood flow drawing different blood cells like WBC etc. in/around the joints.
Meanwhile, a redistribution of arteriolar flow produces stasis and hypoxia at the site of injury.
The resultant localized infiltration of tissues by leukocytes, plasma proteins, and fluid causes the red, swollen, and painful lesions characteristic of inflammation.
Inflammation serves several practical purposes. The influx of leukocytes facilitates the process of phagocytosis, by which damaged cells and other particulate matter are removed from the site of injury. Pain and tenderness serve to remind the sufferer to guard and protect the damaged part, so that the process of repair may be completed without interruption.
Inflammation of a joint may be the outcome of an isolated injury, or it may be a cumulative process that occurs in response to one or more of the following conditions below.
Some of the recognized causes of inflammatory lesions are,
Inflammatory Arthritis (Rheumatoid Arthritis,Spodyloarthropathies)
Osteoarthritis or Degenerative joint disease (primary or secondary)
Connective tissue disease (acquired)
Non-articular rheumatism (tendonitis,bursitis)
Arthritis due to infection
Traumatic or neurogenic disorder
Neoplasm
Rheumatoid Arthritis
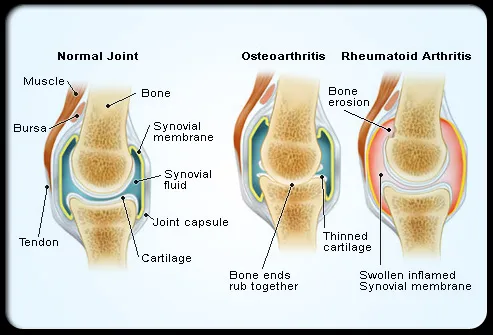
Rheumatoid arthritis (RA) is a chronic autoimmune and inflammatory disease that causes pain, swelling, and stiffness in the joints. RA affects the hands and feet joints on both sides of the body, distinguishing it from other forms of arthritis. It leads to bone erosion and joint deformity. The disease may also affect many other body systems, such as skin, lungs, eyes, nerves, heart, and blood vessels.
Causes Of Rheumatoid Arthritis In rheumatoid arthritis, the body’s natural defense system confuses healthy cells of joint lining with abnormal body cells and attacks them. It is usually the inflammation associated with RA that damages joints and other areas associated. The exact cause of this disease is not known, although genetics appears to play a role. People with certain genes are more likely to have rheumatoid arthritis after a particular viral or bacterial infection. Other risk factors include being a woman, middle or old age, family history, smoking, and obesity.
Causes Of Rheumatoid Arthritis In rheumatoid arthritis, the body’s natural defense system confuses healthy cells of joint lining with abnormal body cells and attacks them. It is usually the inflammation associated with RA that damages joints and other areas associated. The exact cause of this disease is not known, although genetics appears to play a role. People with certain genes are more likely to have rheumatoid arthritis after a particular viral or bacterial infection. Other risk factors include being a woman, middle or old age, family history, smoking, and obesity.

Interventions
- Surgical options like osteotomy, arthroplasty, and joint replacement are considered in patients having very severe symptoms and once the medical line of treatment and interventions have failed. But surgical options should be delayed as much because the total joint arthroplasty might last between 10-20 years. Patients will have to modify his/her lifestyle to a certain extent because of the ergonomics of the replaced joint.
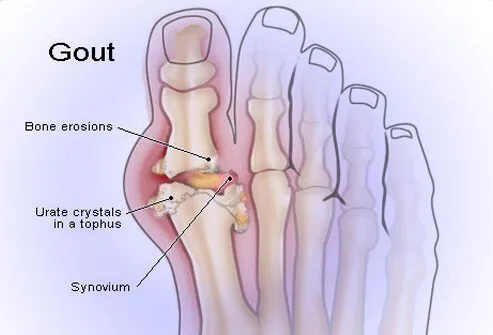
Gout
Gout is metabolic cause of arthritis which arises from mismanagement of some protein metabolism. Gout is a common and complex form of arthritis that can affect anyone. It’s characterized by sudden, severe attacks of pain, swelling, redness and tenderness in one or more joints, most often in the big toe.
An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire. Gout symptoms may come and go, but there are ways to manage symptoms and prevent flares.