Knee Pain

PRP Knee Injection Before And After
Common Causes Of Knee Pain
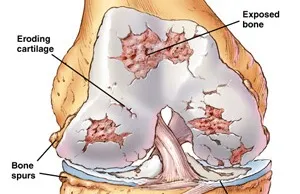
The exact etiology is not known. By chemical stress on articular cartilage and subchondral bone leads to wear and tear to these structures. Thus, joint inflammation is very minimum compared to other arthritis and seen mostly in advanced disease. However, pain of osteoarthritis may be due to the following reasons:
Pain around the joint that increases with weight bearing and movement and improves with rest is the commonest presenting symptom. It may be associated with morning stiffness and swelling of the joints. Clinical signs are tenderness, crepitus, joint effusion, decreased range of movement, valgus/varus deformity etc. X-ray shows decreased joint space, osteophytes formation (bone spur) and osteoporosis of subchondral bone.
Rheumatoid arthritis: Rheumatoid arthritis can affect joints on both sides of the body (both knees, both hands and/or both wrists). In rheumatoid arthritis, your body’s cells attack your own tissues. Rheumatoid arthritis affects three to five times more women than men and often presents between the ages of 20 and 50.
Over time, rheumatoid arthritis can cause cartilage to wear away, swelling in the synovium, and excess fluid in the knee. In later stages, bones can rub against each other.
Bursitis: Bursitis is the inflammation of any of the fluid-filled sacs (bursae) protecting the body’s joints. This is usually caused by repetitive motions or by a stress such as kneeling. Sometimes, a sudden injury can cause bursitis.
Tendonitis: The tendons – rope-like tissues connecting muscles to bone at the knee and other joints – can become painfully inflamed by repetitive and strenuous movement. Tendonitis is a common sports injury, caused by overuse of the same parts of the body. Patellar tendinitis, or “jumper’s knee,” is an inflammation or irritation of the tendon between the knee cap and the shin bone.
Patellofemoral pain syndrome (PFPS): Knee pain or discomfort while walking up and down stairs, jumping or squatting may be symptoms of patellofemoral pain syndrome. This common knee problem is felt toward the front of the knee. It can cause a grinding sensation when bending or straightening your leg, and can cause the knee to occasionally buckle. Sometimes called “runner’s knee,” patellofemoral pain syndrome may be caused by a kneecap that is not aligned properly, overuse, injury, excess weight or when the cartilage in the knee cap is worn significantly.
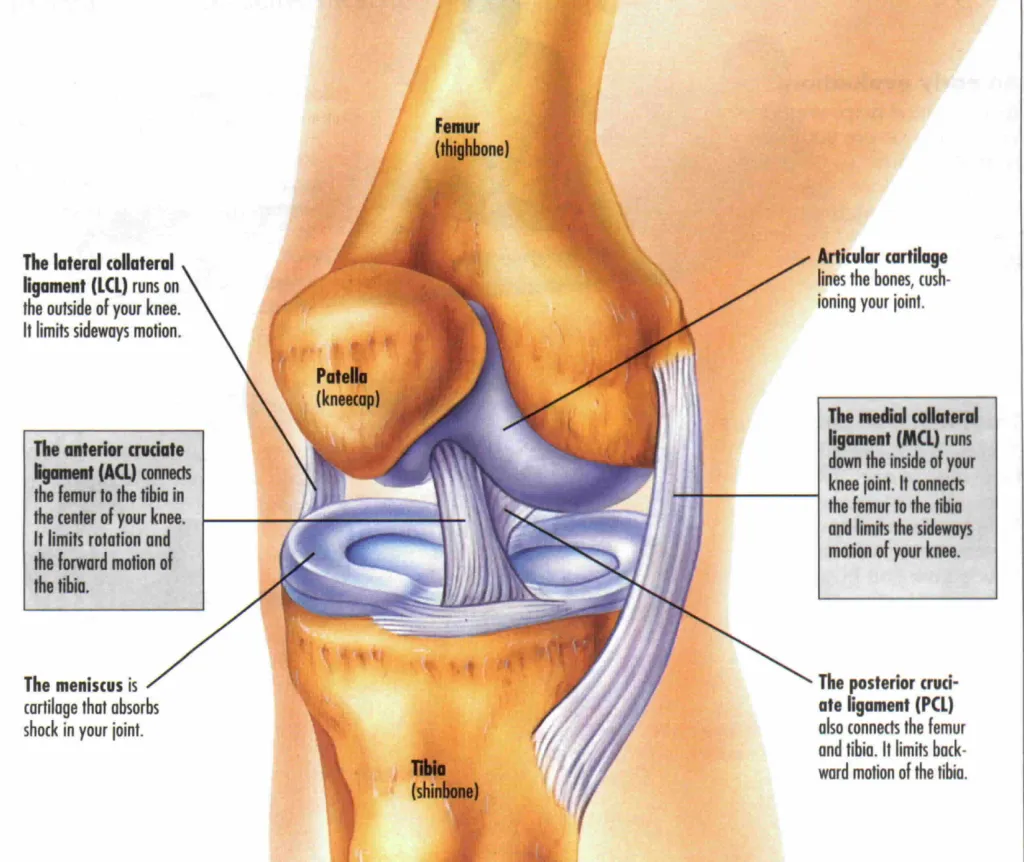
Injuries: Knee injuries can be the result of sports, falls or trauma. They typically involve the ligaments that hold two of the bones of the knee – the femur and tibia – together eg-ACL, MCL, & Meniscal injuries.
Careful medical history which includes:
X-rays, Sonography, MRI, CT Scan
Blood Investigations – Depending upon the history and examination one can be prescribed for blood investigations like Uric Acid, Rheumatoid factor, Anti CCP antibody, Anti Nuclear Antibody, CBC, CRP, Vitamin B12, Vitamin D, Calcium, etc.
TreatmentI. Non-pharmacological therapy

